Oral Presentation The Annual Scientific Meeting of the Australian Diabetes Society and the Australian Diabetes Educators Association 2013
Acute-community collaboration strengthens services for people with complex Diabetes. (#17)
Background:
The HARP Diabetes Co-Management Service (DCS) commenced in 2002. It established Diabetes Nurse Educators in General Practices to support the management of patients with complex diabetes and reduce their risk of hospitalisation. However, throughout this period there has been a dramatic increase in the prevalence of diabetes in hospitalised patients (in 2012 at RMH this was 30% of patients), and of these the complex clients were not offered access to the management of DCS and the extended suite of chronic disease management and support programs provided by HARP.
Aims:
1. To expand the DCS model of care to support the complex diabetes patients who frequent RMH, maintain its community base and GP linkages and establish strong clinical links with the acute hospital.
2. To quantify and examine the characteristics of this complex patient group.
Method:
A DCS DNE was located in the RMH Diabetes and Endocrinology Department to assess and recruit complex Diabetes patients, supported by the RMH HARP Liaison staff. Patients received ongoing care from community based HARP DNEs and associated services. Patients were assessed for complexity utilising the Western HARP Diabetes Prioritisation tool.
Results:
From October 2012 to April 2013, 195 RMH clients were referred to DCS. Of these 102 received services in the community. Referrals from RMH to DCS increased by 38%.
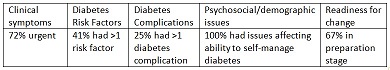
Patients accepted by DCS had the following characteristics:
Conclusion:
This collaboration between the community providers and the RMH Department of Diabetes and Endocrinology addresses a critical clinical need for improved community management for the increasing cohort of people with complex diabetes and associated needs.